
It’s weird in a lot of ways and I feel like a split personality sometimes when working with my patients. I don’t think I will ever lose the experience from the patient side of me, but I can see the clinician in my thinking more and more. I am amazed at the complexities of thoughts on my new side of the therapy table, as the therapist. I am thinking far more things than I can possibly tell you, my patient. My books tell me the basics, and my experience guides me, but YOU, the patient… YOUR stories tell me the most. Now maybe this is unusual, maybe this isn’t the way every therapist works, but it is the way I work! I listen, I watch, I ask my patients questions about what they are feeling and experiencing AND I ask my mentors about what I am seeing and pair the two. All this information tells me things and advises my treatment choices.
The one thing I know for sure is every patient has expectations of their therapist and every therapist has expectations of their patient. When those expectations go unspoken issues result… just like ANY relationship! I’d like to share some of the basic things I see from my new perspective.
What I expect as your therapist:

1. You’re DOING your at-home program!
There are 168 hours in a week. I see you for MAYBE 3 of them. You can NOT get better in 3 hours a week.
My role is to partner with you to help you help yourself. I have no magic wands, no hidden genies and I am not a miracle worker. I often wish I was, and that I could heal you with a flick of my wrist and a Bibbidi Bobbidi boo… but I can’t. No one can. I have no control over how you sit, stand, sleep, or what you chose to do or not do during your day, what you eat, if you do your exercises or not…. only YOU have control over that. I also have no say in how you frame your recovery. Your state of mind is pretty important and while I can help encourage you, I can’t make you believe in yourself. I promise you that I will always be honest and tell you what I know and help where I can, but I am a limited human being. I know what I know and I am committed to learning more, but what I know right now may not be as helpful to you as I want it to be. Might not be what you want to hear, but I promise you I am doing my best to give you the best care I possibly can based on what I know and have experienced. As is every other therapist I have ever met.
2. I expect you to understand therapy isn’t always going to be pain-free.
My job is to help you build muscle to support the movement. Building muscle is HARD WORK. In order to get you back to the life and activities you love… we are going to have some blood sweat and tears. The longer you have been in pain and the longer you have been unable to move the more time this is going to take. Every therapist has a view on how to best deal with this… a starting place if you will and they go from there. DON”T fire your therapist because you hurt. TALK TO THEM.
You have no idea what changes I can make in our plan if you talk to me. After you see me, you will probably be sore. If I am massaging you or you are doing walking lunges…. soft tissue work and therapeutic exercises can BOTH hurt. I expect that. I expect it to be hard, for you to be frustrated as we start more challenging activities. I expect you to tell me the truth when I ask how you are doing or if you’re experiencing increased pain. If you don’t know how to talk to me about that or how to judge it tell me! My expectations are you should be tired and need to rest and might even have increased pain for 24 hours after seeing me. But I expect that pain to go away not linger on and hold you back. There is a dance to therapy and it’s my job to help you balance that dance. So please, answer my questions honestly. I even expect you to not feel like you’re making progress from time to time.
That’s when I get to be your cheerleader and SHOW YOU how far you have come. Trust me. I won’t lie to you. It doesn’t help either one of us. At the same time, I may have to tell you we aren’t making progress. That will be hard to hear. You won’t like it. You will have worked as hard as you can and so will I… it will mean we need another plan, and I may have used every resource I have to help you and might not be able to get you where you need to be. I am committed to doing my best to give you ideas and resources when I have reached the end of my ability to help you. Please understand this does not mean you have failed. It means you need to continue on your journey and possibly try other interventions or need a different approach to your problem. Each therapist will have a different skill set and personality… not everyone will mesh and that’s ok.
3. I can’t fix you in 3 or 4 sessions.
You’ve been in pain for more than 6 months, probably a lot longer before you find a PT. You now have chronic pain. I am sorry. I am, I’ve lived it. But again, PT isn’t magic. I can help you learn to manage your pain… this will be a process and will probably involve more than just me. We can’t really start the heavy lifting until that pain is managed. We have to rebuild you from the inner core out. There’s a lot to it ya know. And as you start living again… dollars to doughnuts more body parts start to ache and hurt. You can tell me when your worried. I am probably expecting it, or can explain why I think it’s happening if your afraid. But know it doesn’t necessarily mean your broken or that therapy isn’t working. In fact it probably means it is. So commit to the process ok. Most likely we will tell you we are going try 4-8 weeks of therapy and reassess then. If you haven’t met any of the goals that were set, there’s a problem. If you have met some, that’s good. Be sure you speak with your PT about what those goals are! For what it’s worth there are people out there that say they can fix you in 3 sessions…. maybe they can. If they do please let me know who so I can learn more!
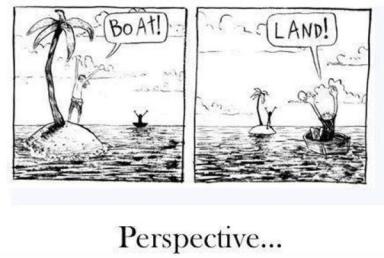
4. The diagnosis you get in therapy is DIFFERENT from your MD diagnosis.
In the world of SI joint pain, this is IMPORTANT to understand. Your MD is going to look at scans and images and blood tests… Your PT is going to look at movement and muscle and function. Just because the names aren’t the same does NOT mean one is right and the other is wrong. We speak different languages and that is just the way it goes. So please, don’t be upset with me if you should ask and my answer is different than your MD’s. What’s written down on paper may or may not match what you think it should, but that does not mean we don’t agree. It means I am doing my job. I understand you want a name for your pain, but isn’t it more important that we are working to manage it successfully?! The language of SI joint pain and dysfunction is hardly standardized. So what I call one thing another therapist or MD might call another. The important part is I am working with you to make your life better…. please understand your MDs and I do not speak the same language, we are specialists in our own right. Physical Therapy is the specialist of the musculoskeletal system. We know rehab, it’s what our profession exists for and is committed to. I promise you, your MD does not know as much about therapeutic exercise as your PT does. On the other hand, I promise not to read your blood tests ok! The best approach is a team approach to managing SI joint pain. Each player on that team is going to have their own language and thoughts. When you blend it all together, that’s when you get the best care and best understanding of how to get better. Each of us sees the elephant from a different angle! Sadly, you’re the one that has to put it all together… but there are resources out there for you.

5. There is no ONE “BEST” way to “fix” Si joint pain and dysfunction.
Do you know there are literally hundreds of classes a therapist can take on the SI joint after they graduate as continuing education? It’s considered an advanced skill and only touched on in school… Each therapist will have their own understanding and approach to treatment. If the one you are working with isn’t a good fit… no harm no foul, try a new one! Each school of thought will reach someone, so it’s ok to look around, call around, and interview your therapist before you head in. In reality, to help with this pain it’s going to take a village. There is NOTHING related to the SI joint that is hard and fast and 100% as far as research goes, so you have to decide what you think and find providers that can help you in the way you think you need help, or you trust to guide you. That’s part of what makes this so hard… the book is BEING written as we all live and breathe. The definition of SI joint pain/ dysfunction isn’t uniform between therapists much less between specialties, research is young and limited, and even the diagnosis of the dysfunction is limited and controversial! Here is a quick and dirty version of how the average specialist will see your SI joint pain.
pain management:tends to see the issue as a problem of pain pathways – hence all the injections and nerve numbing
orthopedic surgeons: see it as a bone-on-bone problem – that’s why you have arthritis and inflammation… fix it with surgery.
chiropractic care:- bones are out of alignment put them back and muscle issues will be fixed
physical therapy – depending on what TYPE of therapist:
pelvic floor
pubic symphysis
muscles pulling bone
bone pulling muscle
ligament laxity
problem in posture
on and on really…..
Massage therapy: tight muscles must be released before your body will move right
prolotherapist: ligament problem too lax… inject them to get them to lay down new tissue and that will stop your pain and make your pelvic girdle stronger.
Then you have people that think if you eat clean and are posture conscious you can fix this… or even just thinking positively and the pain is from emotional trauma.
The list of approaches is endless, and truth be told I think they are all right to a point and each has a piece of that elephant! If it were as easy as one of these specialties being 100% correct we would all be fixed and I wouldn’t be writing this blog, nor would the bunches of others that write on this topic, we would HAVE an answer.
Each approach works differently for different people, and that’s ok! Keep looking for what works for you. Keep an open mind, be flexible be open, and realize whatever you chose as your treatment approach it will take time and effort to see a difference. No matter what the “experts” tell you.


